When I first switched to eating a healthier, plant-based diet I continued to eat fish. I believed I was doing my body good by doing this. After all, fish are rich in omega-3 fatty acids, and omega-3 fatty acids have anti-inflammatory effects on our body. Why wouldn’t I want this?
What I didn’t realize is how many unhealthy substances were in fish, and how these harmful substances have the potential to negatively affect my body and my future health.
This information is important for everyone to know because you can’t just focus on one ingredient in food—especially if this ingredient appears to do good things for you—and forget about the rest of the story if your goal is to improve your overall health. If this were the case, then you could just adopt a diet consisting mainly of Pop-Tarts—being that they’re a “good source” of B-vitamins—and your health would miraculously improve and stay forever perfect. But we all know it doesn’t work like that, and so goes the story with fish.
Let’s take a closer look at the big picture when it comes to our health and eating fish.
The Good on Fish Consumption
As I mentioned, fish are an excellent source of omega-3 fatty acids—an essential fat that has anti-inflammatory properties. Omega-3’s are considered ‘essential’ because your body cannot produce them on its own.[1] They must come from dietary sources. The parent omega-3 fatty acid is known as alpha-linolenic acid (ALA). ALA is the only essential omega-3 fatty acid required from the diet. It can be metabolically converted in humans to the long-chain omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
EPA and DHA are the omega-3’s that people commonly refer to as the “good fats” when consuming fish. Fish get EPA and DHA from eating algae. Humans then get EPA and DHA from eating the fish. Fish are simply the middleman between algae and humans.
The Story of Vegans and Omega-3 Fatty Acid Intake
You may have heard that vegans (people who exclude all animal products from their diets, including fish) cannot convert enough ALA into EPA and DHA to meet the body’s needs and, therefore, it is important that they include fish in their diet or supplement with fish oil. This is not necessarily true, as pointed out in a 2006 article published in the American Journal of Clinical Nutrition:
Several case studies involving n−3-deficient patients reported that intervention with ALA results in marked increases in plasma concentrations of both EPA and DHA. In addition, vegans who consume ALA but not EPA and DHA in their diets have low but stable concentrations of DHA in plasma. Together, these findings suggest that humans can convert meaningful quantities of ALA to EPA and DHA, particularly in the presence of a deficiency or a background of low n−6 fatty acids.[1]
In other words, if you are a vegan, eating a healthy diet with a low omega-6 fatty acid content then you likely have sufficient quantities of the long-chain omega-3 fatty acids available. Low omega-6 fatty acid content is the key here, as this statement is effectively saying a diet devoid of not just animal foods, but also junk foods (including vegan and vegetarian versions) is important for humans to effectively convert enough ALA to EPA and DHA. High omega-6 fatty acid intake in the diet results in a lower conversion of ALA to EPA and DHA by up to 40%.[1] The reason for this is because both omega-6 fatty acids and omega-3 fatty acids use the same enzyme for metabolic conversion purposes in the body from their shorter parent chain versions to their longer chain versions (i.e. ALA to EPA and DHA; LA [linoleic acid] to ARA [arachidonic acid]). Higher amounts of omega-6 fatty acids effectively win the battle for the use of this enzyme. Hence, the importance of eating a whole foods, plant-based diet, free of both animal foods and processed foods, to prevent this from happening.
Getting back to the topic at hand though, fish can still be a rich source of EPA and DHA in the diet for those who prefer to obtain omega-3’s this way.
Dietary Requirements for Omega-3 Fatty Acids
Minimum dietary requirements for ALA—set by the Institute of Medicine—equal 1.1 gm/day for women and 1.6 gm/day for men aged 19-50 years old, 10% of which can come from EPA or DHA.[2] In addition, dietary recommendations of 0.5-1 gm/day of EPA and DHA have been suggested for cardiovascular disease prevention and treatment. Cardiovascular protective effects are also seen with dietary ALA consumption. These protective effects were seen in potentially increasing amounts as you go from 0.58 gm/day to 2.81 gm/day.
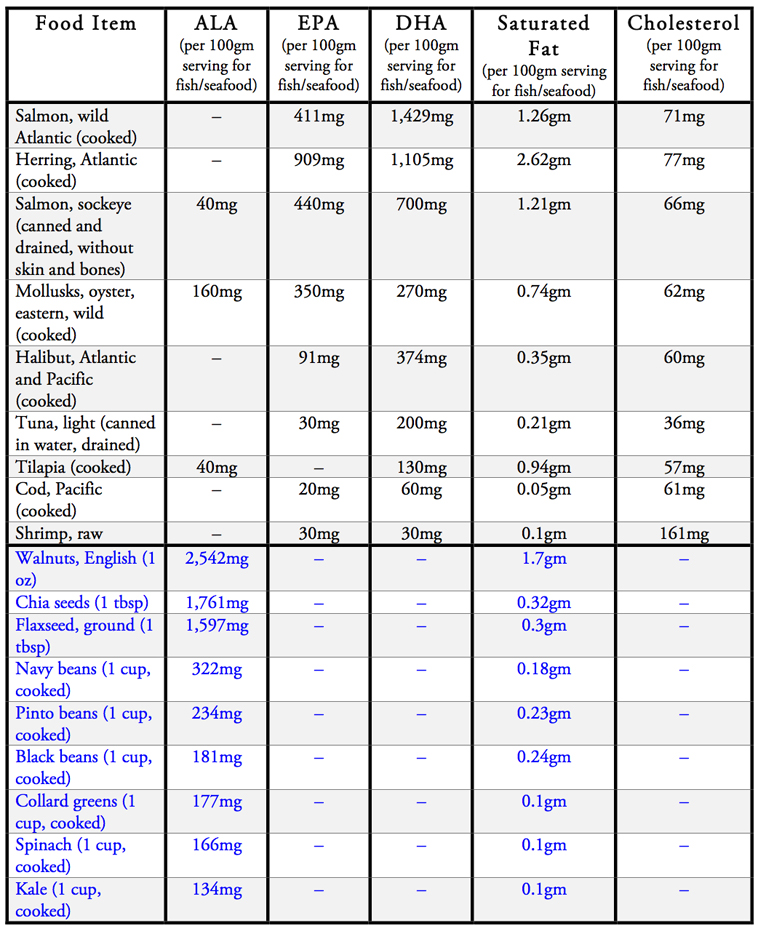
With this in mind, take a look at the table below which summarizes the amounts of omega-3 fatty acids, saturated fats, and cholesterol in different types of food.[3][4] A 100-gram serving of fish is equivalent to a 3.5 ounce portion size.
The Bad on Fish Consumption
While fish may be a rich source of omega-3 fatty acids they are also packaged along with several other harmful substances to human health. The most harmful of these being saturated fat. Additionally, cholesterol, polychlorinated biphenyls (PCBs), dioxins, and mercury round out the other handful of harmful substances found in fish and seafood.
Saturated Fat and Cholesterol
Saturated fat has long been linked to cardiovascular disease. It is known to increase both LDL “bad” cholesterol and total cholesterol levels.[5] In fact, replacing just 5% of energy from saturated fat with the same amount of energy from polyunsaturated fatty acids (omega-3’s fall into this category), monounsaturated fatty acids, or carbohydrates from whole grains can reduce one’s risk of coronary heart disease by 25%, 15%, and 9%, respectively.[6]
High saturated fat consumption also worsens blood pressure. It has been shown that by decreasing saturated fat and increasing monounsaturated fat in the diet a reduction in blood pressure can be obtained.[7]
Dietary cholesterol is found in marine animals, as well as all animal foods, while measurable amounts are completely absent in all plant foods. Please refer back to the chart above for specific amounts of cholesterol and saturated fats found in different foods and species of fish.
Dietary cholesterol raises LDL cholesterol levels in the body, but to a smaller extent than saturated fats do. On average, for every 200 mg of cholesterol consumed per 2,000 calories in the diet a rise in LDL cholesterol between 8 to 10 mg/dl will be seen.[8]
Given the fact that cardiovascular disease is the number one killer in the world, and that saturated fat and cholesterol of animal products play a big role in this, a reduction in both dietary saturated fatty acid and cholesterol would be both prudent and responsible in avoiding this devastating disease.
PCBs, Dioxin, and Mercury
PCBs, dioxin, mercury, and other toxic pollutants also contaminate the fish supply. These agents are environmental poisons having a range of adverse effects, including neurological damage, liver and skin damage, and potential decreased muscle tone and reflexes in infants.[2][10][11] Children are at most risk for these effects, but adults also have the potential to be harmed.
Many farmed Atlantic salmon contain dioxin concentrations that, when consumed at modest rates, pose elevated cancer and noncancer health risks.
In 2004, the Food and Drug Administration and Environmental Protection Agency issued a joint advisory warning to pregnant and nursing mothers, women who may become pregnant, and young children about the toxic effects of mercury from fish consumption.[2] In this advisory they recommend to avoid shark, swordfish, king mackerel, and tilefish altogether due to their high levels of mercury. They also recommend limiting consumption of a variety of other fish including salmon, tuna, shrimp, pollock, and catfish to just 340 grams/week due to mercury accumulation. This is equivalent to approximately 12 ounces of fish per week.
I don’t know about you, but when I hear of any official recommendations to limit the consumption of any food, alarm bells start going off for me. Why else would anyone want to limit any food unless it’s been proven potentially harmful to human health? In contrast, you never hear of any official governmental or professional organizations putting limits on healthy foods like fruits, vegetables, beans, or whole grains. These are the foods that give us life and vibrancy.
There are also organic and inorganic compounds found in fish that have officially been labeled as carcinogenic to humans. These include PCBs, dioxins, toxaphene, dieldrin, and polybrominated diphenyl ethers.[11] The World Health Organization (WHO) provides a tolerable daily intake (TDI) of these substances to help us understand the levels that are potentially toxic to humans. A 2005 study analyzed the levels of these carcinogenic compounds in farmed-raised and wild salmon. Investigators found the following:
Many farmed Atlantic salmon contain dioxin concentrations that, when consumed at modest rates, pose elevated cancer and noncancer health risks. However, dioxin and DLCs are just one suite of many organic and inorganic contaminants and contaminant classes in the tissues of farmed salmon, and the cumulative health risk of exposure to these compounds via consumption of farmed salmon is likely even higher. As we have shown here, modest consumption of farmed salmon contaminated with DLCs raises human exposure levels above the lower end of the WHO TDI, and considerably above background intake levels for adults in the United States.[11]
Both wild and farmed-raised fish contain carcinogens, but it appears that farm-raised fish are even more contaminated than their wild, ocean-living counterparts. Nonetheless, this is just one potential health risk to take into consideration if you’re still considering eating fish.
The Ugly on Fish Consumption
It’s one thing to point out individual harmful components of fish (or any other food substance), and another to evaluate disease, disability, and death rates pertaining to the consumption of these same food items. That’s what we will look at here.
Cardiovascular Disease and Fish Consumption
It is a well-established belief in America and other Western cultures that eating fish protects against heart disease. And, if you were to look only at the surface of this long-held belief then this is exactly what you’ll see—higher fish consumption equals a decrease in heart disease.
However, if you take a deeper look into the scientific literature you’ll find it may not be the fish consumption itself that’s responsible for better heart health. This was apparent when looking at fish consumption in different Mediterranean-style diets as reported in a review article in the European Journal of Clinical Nutrition:
Fish consumption is not positively correlated with ischaemic heart disease mortality. That suggests that dietary factors other than fish, such as the lower meat consumption associated to the higher fish intake, or other differences of lifestyle have perhaps intervened, helping to explain the healthy nature of the Mediterranean diet.[12]
So it was less meat consumption, or perhaps the higher intake of fruits and vegetables, that the Mediterranean diet is known for which is responsible for a reduction in heart disease deaths, not the fish.
The Oxford Vegetarian Study compared vegans, vegetarians, and meat-eaters and their corresponding death rates due to ischemic heart disease.[13] Vegans and vegetarians had less heart disease deaths compared to their meat-eating counterparts. Study investigators also looked specifically at fish consumption in this study and found that “no protective effects were noted for dietary fiber, fish, or alcohol consumption.”
A look at fish consumption in the Iowa Women’s Health Study showed no protective effect in coronary heart disease or stroke mortality.[14]
A study on Danish adults found no benefit with fish consumption and lower coronary heart disease rates on the general population as a whole, but could not exclude a benefit for those at high risk for heart disease.[15]
In another systemic review study in the European Journal of Clinical Nutrition a look at fish consumption in 116,764 individuals found mixed results. Investigators concluded the following:
Fish consumption is not associated with reduced coronary heart disease mortality in low-risk populations. However, fish consumption at 40-60 g daily is associated with markedly reduced coronary heart disease mortality in high-risk populations.[16]
It’s worth pointing out that those typically at high risk of heart disease are also individuals who eat a less healthy diet in the first place, so, like we saw in the Mediterranean diet analysis previously, eating more fish may not be the reason why there is less heart disease seen in these individuals. Instead, less meat or more fruits and veggies could be the reason for the improvement in heart disease and death rates. One really has to look at the big picture in terms of overall dietary changes to see exactly what’s going on here.
Diabetes and Fish Consumption
Diabetes is another disease that official dietary recommendations have encouraged the consumption of fish. But fish consumption does not benefit and may actually worsen type 2 diabetes.[17]
In 2011, a study in the American Journal of Clinical Nutrition followed 36,328 women for an average follow-up period of 12.4 years.[18] Researchers found that as the women ate more fish the incidence of type 2 diabetes increased. The highest intake of fish consumption (≥ 2 servings/day) was associated with the highest rate of type 2 diabetes.
Another review article published in 2014 looked at the prevalence of type 2 diabetes and meat consumption.[19] As individuals went from vegan to vegetarian to pesco-vegetarians to meat eaters the prevalence of type 2 diabetes increased. Vegans had a 2.9% prevalence of type 2 diabetes while pesco-vegetarians (individuals who eat fish but no other meat products) had a 4.8% prevalence of type 2 diabetes. That’s nearly double the rate.
One reason for fish consumption increasing diabetes risk may be the high fat content of marine life. Traditionally, we Americans have believed that fish is a “lean” meat, naturally low in fat. However, this is not the case, as many types of fish have fat content exceeding 20% of total calories.
Why is fat a problem? Because the root cause of type 2 diabetes is excess fat located inside the muscle cells. This causes insulin resistance to develop. So when you eat fatty fish you get fatty muscle cells, and along with fatty muscle cells comes type 2 diabetes.
Summary and Final Conclusions
Popular consensus in our culture glorifies fish and seafood as health-promoting foods. They are not. Marine life is meant to stay in the water where it came from. It’s not for human consumption. At least not if you’re concerned about your health that is.
When you hear about studies claiming health benefits with eating our finned friends, you are most likely hearing about individuals improving their health because they went from worse to bad on the diet spectrum. Going from the Standard American Diet to any diet with less animal products and processed foods will do wonders for the body. So will increasing fruit and vegetable consumption. But eating fish is not healthful.
Currently, there is no scientific evidence showing the addition of fish, to an already healthy diet based on whole plant foods, increases an individual’s health even more. If anything the environmental toxins and saturated fat content in fish and seafood only make it more difficult for the body to ward off disease and illness.
I understand people’s thought processes and desire to improve their diet by eating fish. I, too, was a fish eater myself at one time. It was actually the last meat product I gave up on my journey to adopting a whole foods, plant-based lifestyle. As I learned more about this class of meat though I quickly realized that in order to achieve an optimal state of health, fish had to go. I’m happy to say that I’ve never looked back since ditching my fish habit. Should you decide to make the leap to a fish-free diet, I’m certain you won’t look back either. Your body will be thanking you as well.
Facts About Eating Fish
All fish contain cholesterol, with salmon and shrimp having higher cholesterol in comparison to other seafood
PCBs, dioxin, mercury, and other toxic pollutants contaminate the fish supply
A look at fish consumption in the Iowa Women’s Health Study showed no protective effect in coronary heart disease or stroke mortality
The FDA & EPA issued a joint advisory warning to pregnant and nursing mothers about the toxic effects of mercury from fish consumption
There is no scientific evidence showing the addition of fish to a healthy diet increases an individual’s health even more
References
- Arterburn LM, Hall EB, Oken H. Distribution, interconversion, and dose response of n-3 fatty acids in humans. Am J Clin Nutr. 2006 Jun;83(6 Suppl):1467S-1476S. Review.
- Gebauer SK, Psota TL, Harris WS, Kris-Etherton PM. n-3 fatty acid dietary recommendations and food sources to achieve essentiality and cardiovascular benefits. Am J Clin Nutr. 2006 Jun;83(6 Suppl):1526S-1535S. Review.
- United States Department of Agriculture. National Nutrient Database for Standard Reference Release 21.
- United States Department of Agriculture. National Nutrient Database for Standard Reference Release 28.
- Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Saturated Fatty Acids and Risk of Coronary Heart Disease: Modulation by Replacement Nutrients. Current Atherosclerosis Reports. 2010;12(6):384-390.
- Li Y, Hruby A, Bernstein AM, et al. Saturated Fats Compared With Unsaturated Fats and Sources of Carbohydrates in Relation to Risk of Coronary Heart Disease: A Prospective Cohort Study. J Am Coll Cardiol. 2015;66(14):1538-1548.
- Rasmussen BM, Vessby B, Uusitupa M, et al. Effects of dietary saturated, monounsaturated, and n-3 fatty acids on blood pressure in healthy subjects. Am J Clin Nutr. 2006 Feb;83(2):221-6.
- Institute of Medicine (US) Committee on Diet and Health; Woteki CE, Thomas PR, editors. Eat for Life: The Food and Nutrition Board’s Guide to Reducing Your Risk of Chronic Disease. Washington (DC): National Academies Press (US); 1992. Chapter 6, Fats, Cholesterol, And Chronic Diseases. Available from: http://www.ncbi.nlm.nih.gov/books/NBK235018/.
- Longnecker MP, Rogan WJ, Lucier G. The human health effects of DDT (dichlorodiphenyltrichloroethane) and PCBS (polychlorinated biphenyls) and an overview of organochlorines in public health. Annu Rev Public Health. 1997;18:211-44. Review.
- Liu J, Lewis G. Environmental Toxicity and Poor Cognitive Outcomes in Children and Adults. Journal of environmental health. 2014;76(6):130-138.
- Foran JA, Carpenter DO, Hamilton MC, Knuth BA, Schwager SJ. Risk-Based Consumption Advice for Farmed Atlantic and Wild Pacific Salmon Contaminated with Dioxins and Dioxin-like Compounds. Environmental Health Perspectives. 2005;113(5):552-556.
- García-Closas R, Serra-Majem L, Segura R. Fish consumption, omega-3 fatty acids and the Mediterranean diet. Eur J Clin Nutr. 1993 Sep;47 Suppl 1:S85-90.
- Appleby PN, Thorogood M, Mann JI, Key TJ. The Oxford Vegetarian Study: an overview. Am J Clin Nutr. 1999 Sep;70(3 Suppl):525S-531S.
- Folsom AR, Demissie Z. Fish intake, marine omega-3 fatty acids, and mortality in a cohort of postmenopausal women. Am J Epidemiol. 2004 Nov 15;160(10):1005-10.
- Osler M, Andreasen AH, Hoidrup S. No inverse association between fish consumption and risk of death from all-causes, and incidence of coronary heart disease in middle-aged, Danish adults. J Clin Epidemiol. 2003 Mar;56(3):274-9.
- Marckmann P, Grønbaek M. Fish consumption and coronary heart disease mortality. A systematic review of prospective cohort studies. Eur J Clin Nutr. 1999 Aug;53(8):585-90. Review.
- Kaushik M, Mozaffarian D, Spiegelman D, et al. Long-chain omega-3 fatty acids, fish intake, and the risk of type 2 diabetes mellitus. Am J Clin Nutr. 2009 Sep;90(3):613-20.
- Djoussé L, Gaziano JM, Buring JE, Lee IM. Dietary omega-3 fatty acids and fish consumption and risk of type 2 diabetes. Am J Clin Nutr. 2011 Jan;93(1):143-50.
- Barnard N, Levin S, Trapp C. Meat Consumption as a Risk Factor for Type 2 Diabetes. Nutrients. 2014;6(2):897-910.
Copyright 2024 Center for Nutrition Studies. All rights reserved.
Earn Your Plant-Based Nutrition Certificate
Join over 20,000 students who have improved their health, learned new skills, and even inspired career changes.
Program Overview
- 23,000+ students
- 100% online, learn at your own pace
- No prerequisites
- Continuing education credits