

Autoimmune disorders, including Chron’s disease, type 1 diabetes, multiple sclerosis, and rheumatoid arthritis, affect between 14.7 and 23.5 million people in the U.S., and their incidence may be on the rise.[1]
According to recent research, markers of autoimmunity have increased significantly since 1988, particularly among young people.[2] Women are three times more likely to be affected than men, and autoimmune disease is the eighth leading cause of death among American women ages 15 to 64.[3]
Despite its prevalence, the exact causes of autoimmunity are unknown. However, what scientists and doctors do understand about factors affecting the immune response can provide hope and point the way to relief for sufferers.

What Is Autoimmunity?
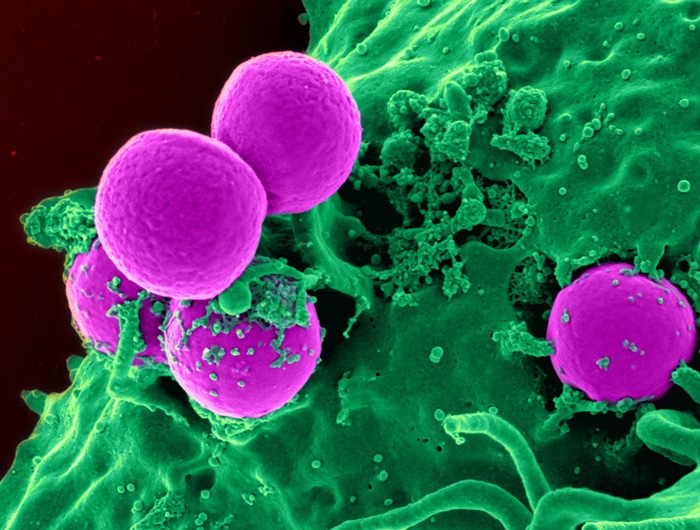
The immune system is designed to recognize the body’s own cells as “self” and pathogens like viruses and bacteria as “non-self.” Immune cells are able to make the distinction thanks to a protein called human leukocyte antigen, which appears on the surface of every “self” cell.
This system breaks down in autoimmune diseases. Instead of leaving “self” cells alone, the body creates autoantibodies that flag native cells as invaders. Autoantibodies can also bind with antigens to create immune complexes, which can trigger a cascade of inflammation that leads to damage and symptoms.[4]
Regulatory immune cells called T-regs are supposed to keep these responses in check but fail to do so in cases of autoimmunity.[5]
Possible Causes of Autoimmune Disease
There’s no single known cause for the immune dysregulation associated with more than 80 different autoimmune diseases, but possible triggers include:[6]
- Genetics.
- Environmental antigens.
- Poor gut health or leaky gut.
- An infection that confuses or disrupts the immune system, causing the body to attack itself.[7]
- Dysfunction in the thymus gland that prevents destruction of autoreactive immune cells.[8]
- Excess of stressors from diet, environment, and/or physical and emotional burdens.
Dietary Autoimmune Triggers
An additional theory, known as “molecular mimicry,” may explain why some foods appear to trigger or exacerbate autoimmune diseases.
For example, elevated levels of immune cells specific to a particular protein in cow’s milk have been discovered in people with type 1 diabetes.[9] The molecular mimicry theory suggests these proteins are similar to proteins in the pancreas, which causes an immune reaction that targets not only the milk proteins but also pancreatic “self” cells.
Other dietary triggers may be related to foods’ effects on gut health. According to one study, additives in highly processed foods may increase intestinal permeability. This can allow antigens and pathogens to pass out of the gut and into the bloodstream, where immune cells subsequently target and attack them.[10] Many of these same foods also affect short-chain fatty acid production in the gut, further contributing to permeability and potentially preventing T-reg cells from maturing properly.[11]
High-sodium diets may also play a role. Salt appears to increase levels of immune cells involved in inflammation and autoimmunity, which makes another case for avoiding highly processed foods.[12] Eating other proinflammatory foods[13] like meat, dairy, and processed vegetable oils puts additional stress on the immune system and may make autoimmune diseases worse.
“Resetting” the Immune System?
Typical autoimmune treatments, such as using NSAIDs or corticosteroids to reduce inflammation, are meant to address symptoms.
But what about dietary change?
Since diet may have a negative effect on autoimmune disease risk and symptoms, is it possible to avoid or control autoimmunity by adopting healthier eating patterns?
Research suggests several reasons why a dietary approach may be worth trying:
- Whole plant foods contain phytonutrients that can act as antioxidants and exert anti-inflammatory effects, which may reduce autoimmune symptoms.[14]
- Using turmeric and ginger to flavor meals can offer additional anti-inflammatory activity.[15]
- Diets that mimic fasting show some promise for suppressing autoimmune responses[16,17] and fighting inflammation.
- Ensuring adequate vitamin D and omega-3 intakes is equated with lower autoimmune disease risk and fewer symptoms.[18]
- Promoting gut health with high-fiber plant foods and probiotics can reduce inflammation in the gut, prevent permeability, and increase short-chain fatty acid production to support healthier immune responses.
Plants are naturally anti-inflammatory and high in fiber, and they contain none of the additives found in highly processed foods.
Whole plant foods are key in maximizing these benefits. Plants are naturally anti-inflammatory and high in fiber, and they contain none of the additives found in highly processed foods. Adjustments may need to be made to remove known allergens or trigger foods, but the diet is flexible and diverse enough to offer options for the majority of people.
While no evidence is yet available to show that diet can “reset“ a dysregulated immune system, eating more plant-based foods is associated with lower levels of inflammation[19] and a more balanced gut immune response.[20]
These factors make a plant-based diet a viable option as part of a protocol to reduce autoimmune symptoms and potentially improve immune function.
References
- The Autoimmune Diseases Coordinating Committee. Progress in autoimmune diseases research. U.S. Department of Health and Human Services (2005).
- Dinse, G. E., Parks, C. G., Weinberg, C. R., Co, C. A. Wilkerson, J., Zeldin, D. C., Chan, E. K. L. & Miller, F. W. “Increasing prevalence of antinuclear antibodies in the United States.” Arthritis Rheumatol 72, no. 6 (2020): 1026–1035. doi:10.1002/art.41214.
- “Autoimmune disease.” National Stem Cell Foundation. https://nationalstemcellfoundation.org/glossary/autoimmune-disease/.
- Elkon, K., & Casali, P. “Nature and functions of autoantibodies.” Nature Clinical Practice Rheumatology> 4, no. 9 (2008): 491–498. doi:10.1038/ncprheum0895.
- “Autoimmune diseases.” Office on Women’s Health. April 1, 2019, https://www.womenshealth.gov/a-z-topics/autoimmune-diseases.
- Campbell, T. “Autoimmune disease: Genes, infection, environment & gut.” Center for Nutrition Studies. March 24, 2020. https://nutritionstudies.org/autoimmune-disease-genes-infection-environment-gut/.
- Orbai, A-Ma. “Autoimmune disease: Why is my immune system attacking itself?” Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/wellness-and-prevention/autoimmune-disease-why-is-my-immune-system-attacking-itself.
- Bauman. Immune & Autoimmune Health Lecture 2. Autoimmunity: Goals & Therapy: Rheumatoid Arthritis, Systemic Lupus Erythematosus. https://baumancollege.org/programs/nutrition-consultant/.
- Chia, J. S. J., McRae, J. L., Kukuljan, S., Woodford, K., Elliott, R. B., Swinburn, B., & Dwyer, K. M. “A1 beta-casein milk protein and other environmental pre-disposing factors for type 1 diabetes.” Nutr Diabetes 7, no. 5 (2017). doi:10.1038/nutd.2017.16.
- Lerner, A., & Matthias, T. “Changes in intestinal tight junction permeability associated with industrial food additives explain the rising incidence of autoimmune disease.” Autoimmunity Rev 14, no. 6 (2015): 479–489. doi:10.1016/j.autrev.2015.01.009.
- Haghikia, A., Jörg, S., Duscha, A., Berg, J., Manzel, A., Waschbisch, A., Hammer, A., Lee, D-H, May, C. Wilck, N., Balogh, A., Ostermann, A. I., Schebb, N. H., Akkad, D. A., Grohme, D. A., Kleinewietfeld, M., Kempa, S., Thöne, J., Demir, S., Müller, D. N., Gold, R., & Linker, R. A. “Dietary fatty acids directly impact central nervous system autoimmunity via the small intestine.” Immunity 44, no. 4 (2016): 951–953. doi:10.1016/j.immuni.2016.04.006.
- Greger, M. “One way to treat asthma and autoimmune diseases with diet.” NutritionFacts.org. June 16, 2020. https://nutritionfacts.org/2020/06/16/one-way-to-treat-asthma-and-autoimmune-diseases-with-diet/.
- Freuman, T. D. “Your anti-inflammatory diet is probably just the opposite.” U.S. News & World Report. https://health.usnews.com/health-news/blogs/eat-run/articles/2018-10-11/your-anti-inflammatory-diet-is-probably-just-the-opposite.
- Yahfoufi, N., Alsadi, N., Jambi, M. & Matar, C. “The immunomodulatory and anti-inflammatory role of polyphenols.” Nutrients 10, no. 11 (2018): 1618. doi:10.3390/nu10111618.
- “Autoimmune disease.” DrFuhrman.com. https://www.drfuhrman.com/health-concerns/6/autoimmune-disease.
- Choi, I. Y., Lee, C., & Longo, V. D. “Nutrition and fasting mimicking diets in the prevention and treatment of autoimmune diseases and immunosenescence.” Mol Cell Endocrinol 455 (2017): 4–12. doi:10.1016/j.mce.2017.01.042.
- Choi, I. Y., Piccio, L., Childress, P., Bollman, B., Ghosh, A., Brandhorst, S., Suarez, J., Michalsen, A., Cross, A. H., Morgan, T. E., Wei, M., Paul, F., Bock, M. & Longo, V. D. “A diet mimicking fasting promotes regeneration and reduces autoimmunity and multiple sclerosis symptoms.” Cell Rep 15, no. 10 (2016): 2136–2146. doi:10.1016/j.celrep.2016.05.009.
- “Is there a link between nutrition and autoimmune disease?” Today’s Dietitian. https://www.todaysdietitian.com/newarchives/110211p36.shtml.
- Craddock, J. C., Neale E. P., Peoples, G. E., & Probst, Y. C.. “Vegetarian-based dietary patterns and their relation with inflammatory and immune biomarkers: A systematic review and meta-analysis.” Advances in Nutrition 10, no. 3 (2019): 433–451. doi:10.1093/advances/nmy103.
- Zhang, C., Björkman, A., Cai, K., Liu, G., Wang, C., Li Y., Xia, H., Sun, L., Kristiansen, K., Wang, J., Han, J., Hammarström, L., & Pan-Hammarström, Q. “Impact of a 3-months vegetarian diet on the gut microbiota and immune repertoire.” Front Immunol 9 (2018). doi:10.3389/fimmu.2018.00908.
Copyright 2025 Center for Nutrition Studies. All rights reserved.
Deepen Your Knowledge With Our
Plant-Based Nutrition
Certificate
Plant-Based Nutrition Certificate
- 23,000+ students
- 100% online, learn at your own pace
- No prerequisites
- Continuing education credits







