In this article, I explore what cutting-edge preclinical research on cancer looks like today and what we can learn from viewing it through the lens of Dr. Campbell’s research on cancer.
Clearly, many things have changed in the nearly fifty years since Congress passed the National Cancer Act of 1971. But what concerns me most are the things that have not changed. Cancer remains a leading cause of death. Advances across all biomedical sciences continue to astound, and have contributed greatly to increasing “the present state of our understanding,” but what benefits have we reaped from that understanding? Our ability to treat cancer has not improved, despite an extraordinary amount of resources dedicated to this mission. Last and most important, nutrition remains as undervalued and underutilized now as it was back then.
T. Colin Campbell, The Future of Nutrition, p. 27
In 2020, the US spent over $200 billion on cancer care, with costs expected to increase to $245 billion by 2030.[1] This astonishing number does not include the vast sums spent on research. The US cancer research budgets of pharmaceutical companies were estimated at more than $46 billion in 2021,[2] plus the annual $7.3 billion budget allocated by Congress to the National Cancer Institute (NCI). Large amounts of philanthropic funding also support cancer research; according to a recent article in The Lancet, over $14 billion of US philanthropic funding flowed into cancer research between 2016 and 2020.[3]
There are a few possible reasons why cancer research might cost so much. First, since modern medicine is founded on the local theory of disease, most research focuses on identifying and bringing to market so-called targeted solutions, such as specific drugs for specific forms of cancer.[4] Relatedly, medical research has fully embraced the belief that the randomized, placebo-controlled trial is the only way to reach the truth. This approach, invented for testing drugs, makes for very costly study design. Second, since cancer occurs in different parts of the body, separate research specialties have developed around each “type” of cancer. Each specialty has its own laboratories, hardware and software, teams of experts, medical journals, and funding streams. Third, medical research is heavily focused on treating disease symptoms rather than the root causes. As with all chronic diseases, the symptoms of cancer do not appear overnight but develop slowly over multiple years. Once the human body, arguably the most complex system on earth, has tipped into a disease state, it is much harder and thus more costly to restore health by only treating symptoms. Fourth, because of the belief that advances in modern medical research stem from ever-greater specialization, we have lost sight of the bigger picture and are not tackling the problem in a coordinated, strategic fashion that incorporates everything known about cancer.
If you are familiar with the arguments presented by Dr. Campbell in Whole: Rethinking the Science of Nutrition, you might have noticed that all these reasons are connected to the fact that the vast majority of cancer research is conducted within a reductionist paradigm. Researchers in a reductionist paradigm seek to better understand biological systems by deconstructing complex cellular processes into their parts and to remediate disease by targeting specific elements of these systems in a tightly focused manner.
One example of cutting-edge preclinical cancer research is a recent study from Dr. Jing Chen’s Laboratory at the University of Chicago.[5] This study, published in the prestigious journal Nature, received funding from the NIH and philanthropic donors. It caught our attention at the Center for Nutrition Studies because it appears to connect cancer and nutrition. Indeed, the authors introduce their study by acknowledging that diet has been an important environmental factor during human evolution, shaping both physiological and pathological adaptations, and alluding to “extensive studies on links between diet and human health and disease.”
A Quick Primer on Trans-Vaccenic Acid (TVA)
Before we dive into the study, I need to introduce you to its hero, a trans fatty acid called trans-vaccenic acid. Depicted in two ways below, TVA is one of three naturally occurring trans fatty acids (TFAs, also colloquially described as trans fats). For the chemically curious, it is an unsaturated fatty acid with one trans double bond. (In a trans double bond, the two carbon atoms participating in the double bond are bonded to different groups, and these groups are located on opposite sides of the double bond). With 18 carbon atoms, TVA is classed as a long-chain fatty acid (LCFA). Its chemical formula is C18H34O2.
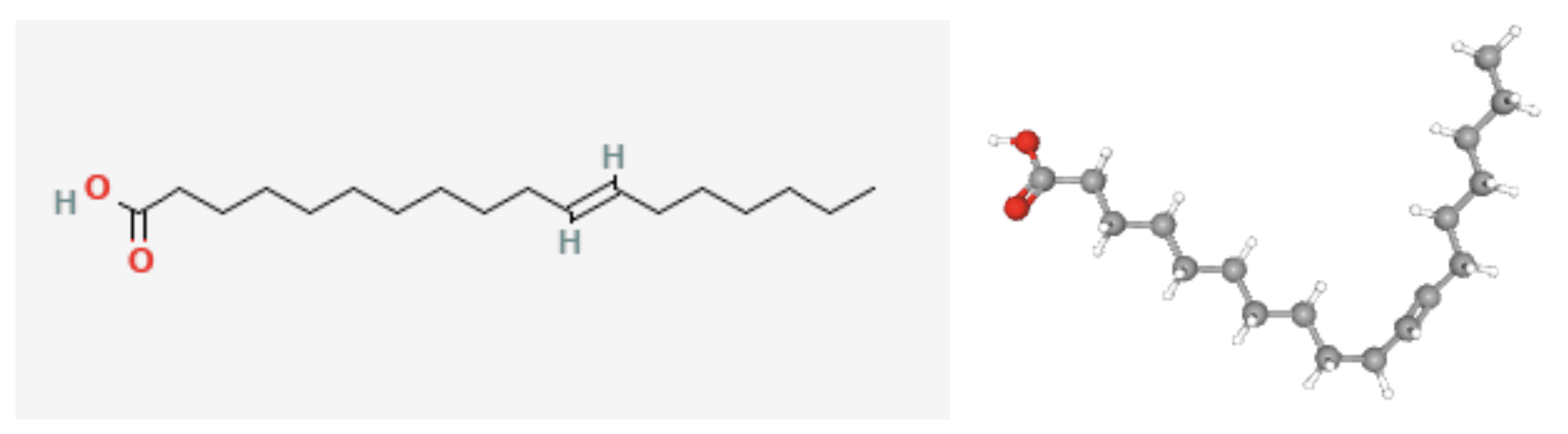
PubChem Identifier: CID 5281127
2D structure & 3D Conformer[6]
Naturally occurring trans fatty acids are found only in animals. Ruminant meat is the richest source of TVA because trans fatty acids are produced by microbial fermentation in the rumen, a specialized chamber of the stomach of cows, sheep, and goats. Indeed, the vaccenic part of the name comes from the Latin vacca, meaning cow. In dairy cows, TFAs produced in the rumen are incorporated into the milk fat during lactation. Consequently, TVA is found in dairy products and the fat of ruminant meat. Cheese, milk, yogurt, burgers, chicken fat, turkey meat, bologna, and hot dogs contain about 1–5% trans fats, most of which are TVA.[7] Human breast milk also often contains TVA as a result of dietary intake.
TFAs in general are widely believed to contribute to the development of certain diseases. A high intake of industrially produced TFAs, which are found in partially hydrogenated vegetable oil, has been shown to negatively affect human health; they are associated with an increase in the level of low-density lipoprotein (LDL-cholesterol, “bad cholesterol”) and a decrease in the level of high-density lipoprotein (HDL-cholesterol, “good cholesterol”), leading to increased risk of heart disease.[8] Recognition of these harms led to mandated labeling and restrictions on their use. Whether natural trans fats such as TVA are linked to the same health concerns is less clear, but some researchers argue that a causal association exists between total TFA intake (industrial plus natural) and increasing risk of heart disease, diabetes, and cancer.[8]
Understanding Cancer Metabolism to Fight Cancer
Jing Chen is a well-known academic researcher in cancer metabolism, an area of molecular biology research that investigates at a very granular level the metabolic alterations that occur in cancer cells and their role in tumor formation and cancer progression. His lab’s work focuses on “elucidating the signaling links between metabolism and cancer for a better understanding of cancer metabolism and improved clinical outcomes.”[9] In other words, they investigate communication pathways connecting metabolic processes with cancer progression; the hope is that they might apply this improved understanding to develop a foundation for new clinical treatments that control tumor growth and eliminate tumor invasion and metastasis.
In what might initially seem like a nod to the importance of diet when treating cancer, Chen’s research has focused recently on understanding how circulating blood chemicals, including nutrients derived from food, affect the immune system’s response to the development, growth, and metastasis of cancer. On closer inspection, however, it becomes clear that his research approach adheres closely to the pharmaceutical playbook (and, I daresay, also appears to share its profit motive).
Rather than examining the impact of different dietary patterns on the immune system’s ability to deter and fight cancer, the Chen lab tests isolated blood chemicals for tumor-fighting ability in the same way that Big Pharma tests individual drug candidates. The goal is to identify chemicals that can be isolated and sold as supplements that may enhance the effectiveness of existing immunotherapies (therapies that seek to harness the power of the immune system to fight cancer).

Trans-Vaccenic Acid to the Rescue?
In November 2023, the Jing Chen lab published a study of breathtaking technical complexity in collaboration with ten other research teams in four universities and research institutes.[5] It identified that, of 255 different blood chemicals tested, TVA may potentially enhance “anti-tumor immunity” and augment the effectiveness of various existing immunotherapies. Researchers demonstrated that:
- In vitro, in both human and mouse cell line models, TVA activates white blood cells called CD8+ T cells and improves their ability to kill cancer cells. (CD8+ T cells are often called “the foot soldiers of the immune system,” because they help the body fight infection and disease.)
- Mouse CD8+ T cells were more effective at reducing cancer development in melanoma tumor-bearing mice fed a TVA-rich diet compared to controls fed a non-TVA-rich diet. (The TVA-rich diet formula contained 1% TVA by weight.)
- In a retrospective clinical study, human patients who responded to a kind of immunotherapy called CAR T-cell therapy had significantly higher circulating TVA in their blood serum than nonresponders.
The researchers were also able to partially uncover how TVA enhances antitumor immunity at the molecular level. They conclude their paper by noting that additional studies are warranted to further elucidate the process and in particular the role of TVA in inactivating a receptor, GPR43, that is typically activated by short-chain fatty acids produced by our gut microbiota. GPR43 activation has a suppressive role in CD8+ T cells; in a healthy body, this activation might serve to limit excessive immune responses. However, if the top priority is to boost CD8+ T cell activity to fight a tumor, one might rather undermine normal GPR43 function. Effectively, by disrupting the GPR43 receptor, TVA allows for an exaggerated CD8+ T cell response.
The chart below, pulled from the Nature paper, illustrates that over 20 days, the melanoma tumors in the mice fed the 1% TVA diet grew half as much as the tumors in the control mice, a rapid and powerful effect; however, since the experiments were stopped at 20 days, it is unclear whether this effect extended the lifespan of the tumor-bearing mice.
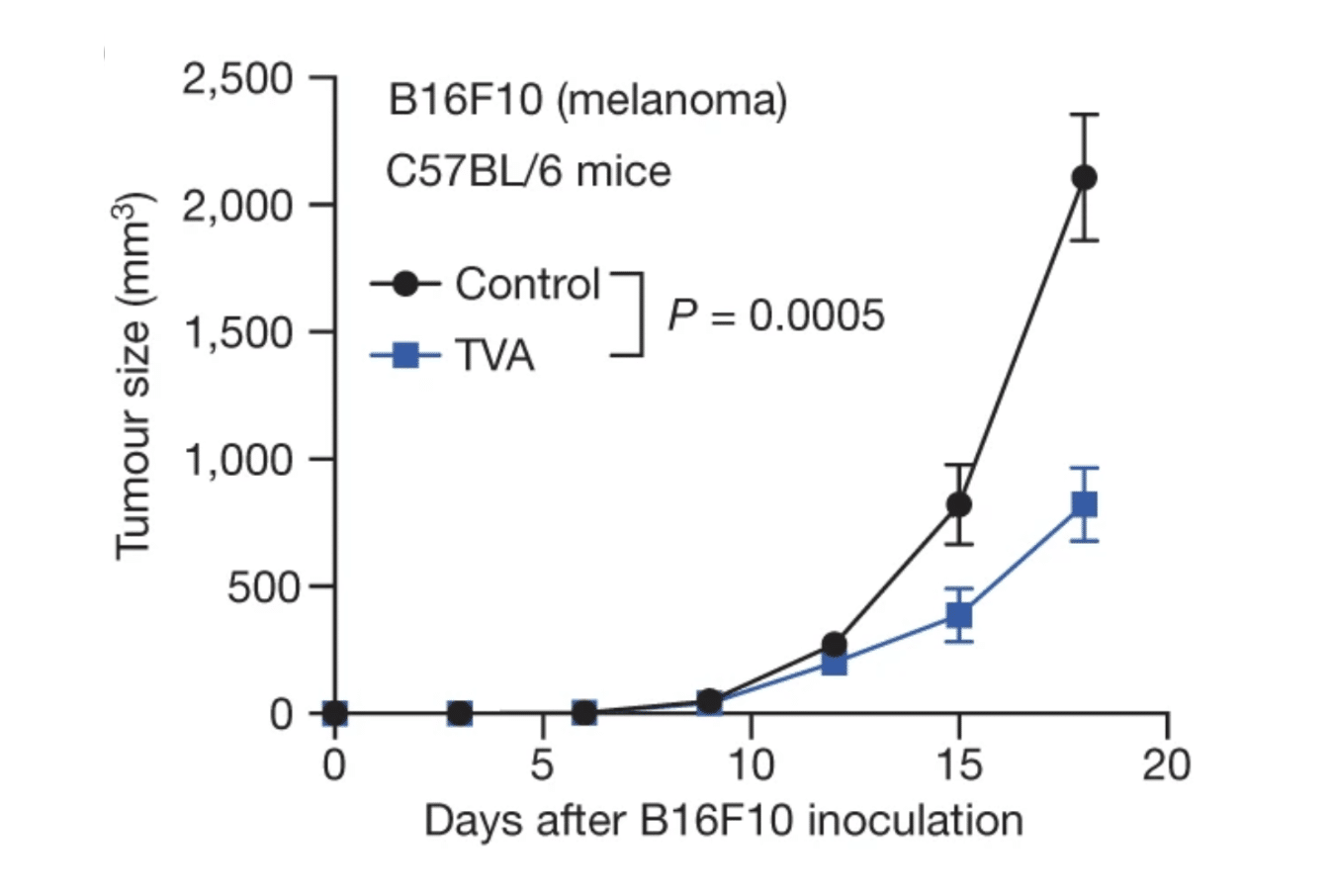
“Fig. 1(b): Dietary TVA enhances anti-tumour immunity through effector CD8+ T cells” by Fan H et al. CC BY 4.0.
The TVA study was huge, involving some 43 authors, and presumably very costly given the highly technical methodology. Given the huge investment of human and institutional resources, it is not surprising that plans exist to commercialize the findings of the study. The disclosure of competing interests at the end of the paper reveals that Jing Chen (JC) has patents pending on TVA and TVA derivatives. Given that TVA is naturally occurring, he would need to demonstrate that he has isolated, purified, or modified it in a way that results in a new and useful composition not achievable in its natural state. (A few other researchers involved in the study also disclosed competing interests, though none appear to be directly related to this specific study.) Thus, in a few years, there may be clinical trials to determine whether increasing dietary TVA intake in cancer patients augments the effectiveness of immunotherapy.
So What Does This Mean? Does It Matter?
Will TVA supplements yield improved immunotherapy outcomes? It is very hard to say for a few reasons:
- We only know that TVA affects a surrogate marker (the CD8+ T cell) of antitumor immunity; the entire tumor suppression pathway is long and complex.
- The relationship between the amount of any nutrient consumed and the amount that the body uses is unpredictable. As Dr. Campbell explains in Whole, on page 69, “supplementation with large doses of discrete nutrients does not guarantee utilization of those nutrients.”
- The history of nutrient supplement research shows that supplements do not produce the same effects as the nutrients in whole foods (in some cases, supplements even behave opposite to whole foods), and supplements have limited usefulness beyond sometimes preventing deficiency.
- There could be unanticipated side effects of administering supplemental TVA, not least because it appears to block the activation by short-chain fatty acids of GPR43 (described above), which modulates various physiological processes, including inflammation, immune responses, energy metabolism, and gut homeostasis.
- We do not know how TVA might interact with other nutrients. The interactions will vary depending on what else patients consume with their TVA supplements. As Dr. Campbell writes in Whole, “Interactions among individual nutrients in food are substantial and dynamic – and have major practical implications. An outstanding review by researchers Karen Kubena and David McMurray at Texas A&M University summarized the published effects of a large number of nutrients on the exceptionally complex immune system.”
One thing seems certain: if clinical trials show TVA can improve the efficacy of immunotherapy and if side effects are manageable, we can expect an explosion in demand for such supplements. This demand will come not only from its use for treating cancer but also from the general public who will likely jump to the conclusion that TVA supplementation may prevent cancer in the first place. Given some of the headlines generated by the study, we might also anticipate increased consumer confusion about the healthfulness of eating meat and dairy.
Reductionism-Fueled Confusion
Have you ever noticed that when experimental animal research reveals a supposed benefit to nutrients from meat and dairy, the research gets attention in the media and people seem willing to believe that the findings are relevant to humans, despite the differences between rodents and humans; however, when experimental animal research shows the benefits of plant-based nutrition, people question its relevance to humans, and the media fail to promote it?
When the TVA paper was published, clickbait headlines, such as the one pictured below, appeared in the lay medical literature, making the huge leap of asserting that consuming red meat and dairy could help prevent cancer. Other headlines included “Nutrient found in beef and dairy improves immune response to cancer” and “UChicago study finds fatty acid found in some red meat can help fight cancer.” Naturally, carnivore advocates had a field day!
Reporting like this contributes to our collective confusion about nutrition. It fuels the beliefs of people who do not want to change their habits, those who insist on the mantra everything is fine in moderation, or those in both camps. I cannot help but wonder who is writing such headlines. Are meat- and dairy-loving media automatons taking over? Perhaps they are. Media outlets are increasingly looking to generative AI tools, built on top of large language models (themselves trained on internet data sources) to churn out news copy, so perhaps we should not be surprised when relatively sober press releases, such as the one released by the University of Chicago following this TVA study, are woefully misinterpreted.[10] The researchers themselves explicitly acknowledge the association between meat intake and the risk of multiple forms of cancer: “Consuming red meat may provide TVA for improved anti-tumour immunity, but a high intake of red meat has been positively associated with risk of many cancers, including breast, colorectal, colon and rectal cancer. Thus, our studies support TVA supplementation as a more targeted and efficient way than dietary changes to benefit anti-tumour immunity.”[5]

It seems whoever (or whatever) wrote these articles was unaware of the evidence showing that a whole food, plant-based (WFPB) diet is best for reducing the risk of cancer.[11] Nor do they appear to have considered how much meat and dairy humans would need to consume to ingest similar levels of TVA as those levels fed to the mice in the study. The concentration of TVA in ruminant meat varies depending on factors such as the fat content of the cut of meat and the animal’s diet and breed, but typical concentrations of TVA in ruminant meat range from 1–5% of total fatty acids. In turn, total fatty acids represent only 5–10% by weight of lean cuts of meat and 15–20% by weight of fattier cuts. That means lean cuts will contain 0.05–0.10% TVA by weight, while fatty cuts will contain 0.75–1.00% TVA by weight. A person would need to eat a diet comprising 100% of the fattiest cuts of meat to achieve an intake of TVA approaching the level (1% by weight) fed to the mice in this study.

What Can We Learn from Revisiting Dr. Campbell’s Experimental Research?
Published data show that a diet high in animal protein promotes tumor growth.[11] Animal protein increases the levels of a hormone, IGF-1, which is a risk factor for cancer, and diets high in casein (the main protein of cow’s milk, but also found in other types of mammalian milk) allow more carcinogens into cells, which allow more dangerous carcinogen products to bind to DNA, which allows more mutagenic reactions that give rise to cancer cells, which allow more rapid growth of tumors once they are initially formed. This is relevant because all the experimental mice in the TVA study were fed a dietary formula containing 20% casein. Why a milk protein is considered suitable for mice is unclear.
It is rather instructive to view this strand of the study through the lens of Dr. Campbell’s research on the impact of dietary protein on cancer development in rats (described in detail in Chapter 3 of The China Study). The charts below are drawn from the book and illustrate the findings of experiments with rats given an initial dose of carcinogen and then fed the different diet formulas indicated on the horizontal axes. Unless otherwise noted, the protein in the diet formula is casein. The charts clearly show a dose-response relationship between cancer development and the level of casein in the diet.
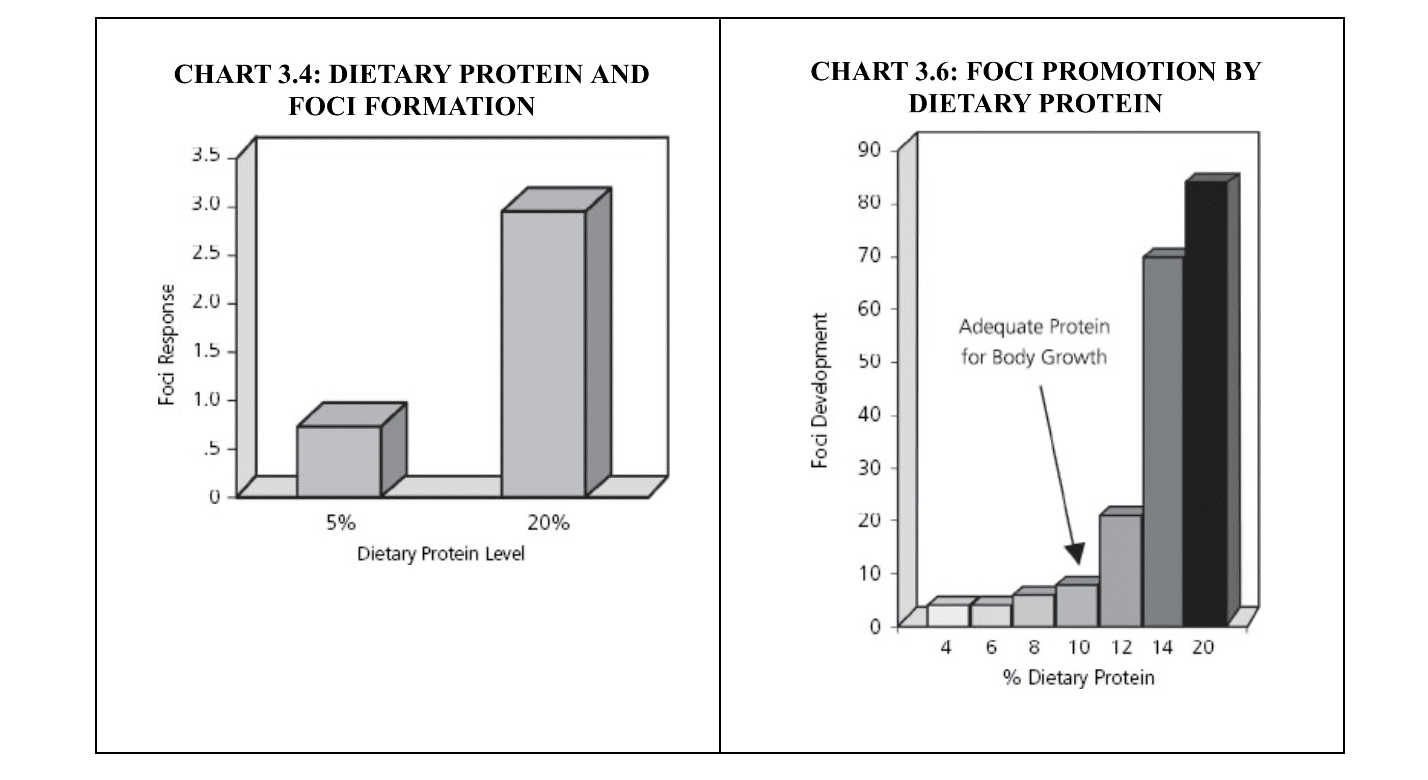
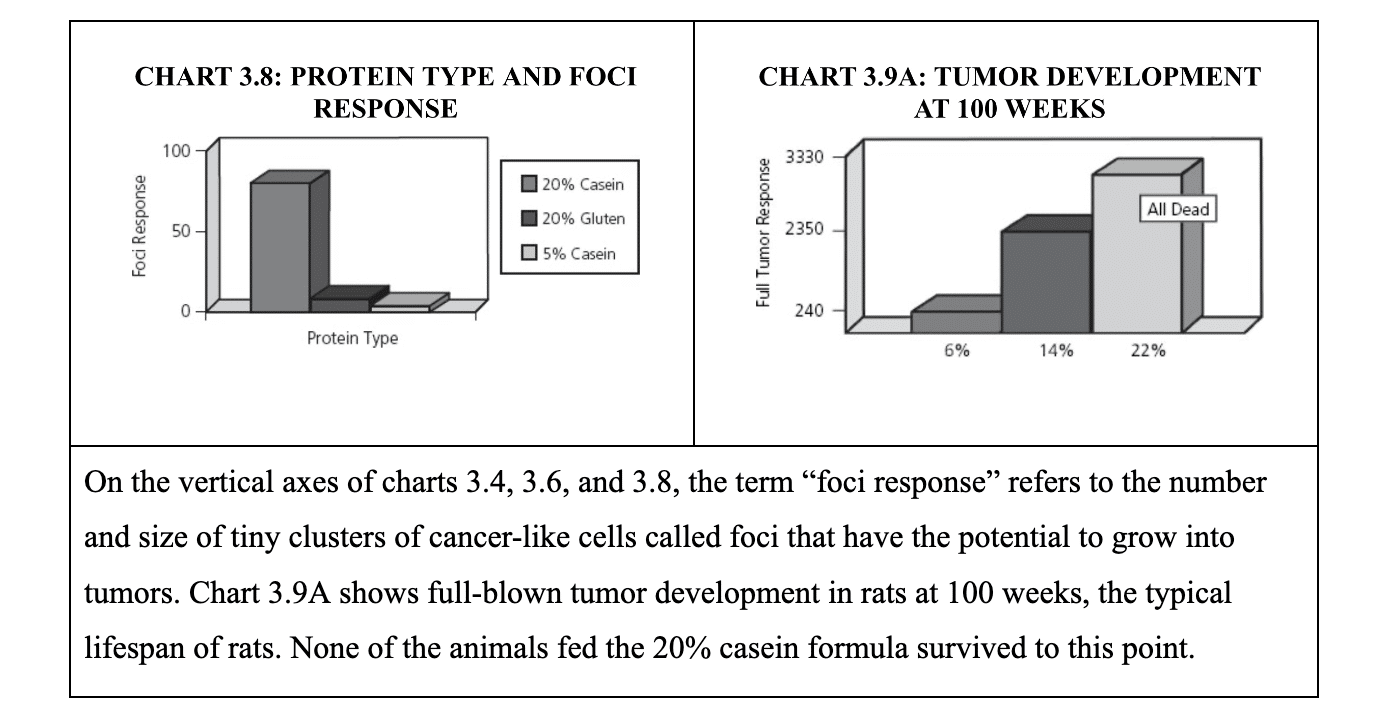
Rats and mice share a common ancestry as members of the order Rodentia and thus have many similarities in terms of genetics and evolutionary history. Presumably the researchers had never come across Dr. Campbell’s work; otherwise, they would have known that their chosen diet formula had previously been shown to promote cancer growth in rats dosed with carcinogens such as aflatoxin and also in mice prone to liver cancer. I cannot help wondering what the TVA study results would have been had the mice been fed a different dietary formula. Perhaps the same or greater effect might have been accomplished merely by making either of the changes that Dr. Campbell has shown to turn off cancer growth in experimental animals: (1) reducing the percent of casein in the diet formula from 20% to 5–6% or (2) substituting a plant-derived protein (gluten or soy) for casein. We will never know unless the TVA experiment is repeated using identical conditions except for the protein in the feed.
Conclusions
As the predominant approach in modern medical research, reductionism has helped significantly improve our understanding of disease.[12] However, as Dr. Campbell eloquently articulated in Whole, there are major downsides to the unchecked pursuit of reductionist research. The big picture recedes from view as research becomes ever more complex and scientific disciplines so specialized that experts can barely understand each other, let alone step back and take in the whole. Symptoms are mistaken for root causes and as a result, we fail to target the root causes of disease. Meanwhile, provocative outlier findings that cannot be filed neatly within existing paradigms in research medicine, such as those of Dr. Campbell, are ignored or dismissed at a huge cost to public health.
The study’s authors state that “little is known about how the circulating diet-derived nutrients affect specific human physiological and pathological processes” and imply that this lack of a molecular-level understanding is holding back progress on deciphering the links between diet and human health and disease. For the reasons explored in this article, this assertion strikes me as both arrogant and revealing of reductionism’s blind spot. A lack of a molecular-level understanding is not holding back progress on deciphering the links between diet and human health and disease. What is holding back progress is the resistance of the medical establishment to break free of the reductionist paradigm and take seriously the ever-growing body of wholistic evidence that demonstrates the beneficial impact of plant-based nutrition and the detrimental effect of diets centered on animal protein on human health. As Dr. Campbell would say, what truly matters is that the WFPB diet works, not how it works at a molecular level.
References
- American Association for Cancer Research (AACR). Cancer care costs in the United States are projected to exceed $245 billion by 2030. June 10, 2020. https://www.aacr.org/about-the-aacr/newsroom/news-releases/cancer-care-costs-in-the-united-states-are-projected-to-exceed-245-billion-by-2030/
- Fried C. Huge spending—but little sharing of research results—on cancer drugs. UCLA Anderson Review. November 15, 2023. https://anderson-review.ucla.edu/huge-spending-but-little-sharing-of-research-results-on-cancer-drugs/
- McIntosh SA, Alam F, Adams L, et al. Global funding for cancer research between 2016 and 2020: a content analysis of public and philanthropic investments. Lancet Oncol. 2023;24(6):636-645. doi:10.1016/S1470-2045(23)00182-1
- Campbell TC. Nutrition and Cancer: An Historical Perspective.-The Past, Present, and Future of Nutrition and Cancer. Part 2. Misunderstanding and Ignoring Nutrition. Nutr Cancer. 2017;69(6):962-968. doi:10.1080/01635581.2017.1339094
- Fan H, Xia S, Xiang J, et al. Trans-vaccenic acid reprograms CD8+ T cells and anti-tumour immunity. Nature. 2023;623(7989):1034-1043. doi:10.1038/s41586-023-06749-3
- National Center for Biotechnology Information. PubChem Compound Summary for CID 5281127, trans-Vaccenic acid. https://pubchem.ncbi.nlm.nih.gov/compound/trans-Vaccenic-acid. Accessed Apr. 11, 2024.
- USDA Agricultural Resource Service (ARS). Fat and fatty acid content of selected foods containing trans-fatty acids. https://www.ars.usda.gov/ARSUserFiles/80400525/Data/Classics/trans_fa.pdf
- Islam MA, Amin MN, Siddiqui SA, Hossain MP, Sultana F, Kabir MR. Trans fatty acids and lipid profile: A serious risk factor to cardiovascular disease, cancer and diabetes. Diabetes Metab Syndr. 2019;13(2):1643-1647. doi:10.1016/j.dsx.2019.03.033
- Dr. Jing Chen laboratory @ UChicago. Our research. Accessed April 13, 2024. https://sites.google.com/view/jingchen-lab-uchicago/home
- Wood M. Nutrient found in beef and dairy improves immune response to cancer. UChicago Biological Sciences Division. November 22, 2023. https://biologicalsciences.uchicago.edu/news/tva-nutrient-cancer-immunity
- Campbell TC. Cancer Prevention and Treatment by Wholistic Nutrition. J Nat Sci. 2017 Oct;3(10):e448. PMID: 29057328; PMCID: PMC5646698. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5646698/#R4
- Beresford MJ. Medical reductionism: lessons from the great philosophers. QJM. 2010;103(9):721-724. doi:10.1093/qjmed/hcq057
Copyright 2026 Center for Nutrition Studies. All rights reserved.
Deepen Your Knowledge With Our
Plant-Based Nutrition
Certificate
Plant-Based Nutrition Certificate
- 23,000+ students
- 100% online, learn at your own pace
- No prerequisites
- Continuing education credits